Injectable Lenacapavir: A New Frontier in HIV Prevention
The launch of injectable lenacapavir (LEN) as an additional pre-exposure prophylaxis (PrEP) option represents a transformative breakthrough in the global effort to curb HIV infections. This long-acting, twice-a-year injectable solution offers a promising alternative to daily oral pills—a change that promises to address several of the tricky parts associated with consistent adherence to traditional regimens. With key populations facing tangled issues like stigma and limited access to health care, LEN ushers in a new chapter in HIV prevention strategies.
The most appealing aspect of LEN is its capacity to simplify protection by replacing daily medication with just two doses per year. This innovation has the potential to reduce adherence challenges and offer greater freedom to those at risk. As health authorities and global partners work together to implement these guidelines, there remains a strategic imperative to ensure that this advancement reaches every community quickly and safely.
Expanding the HIV Prevention Arsenal
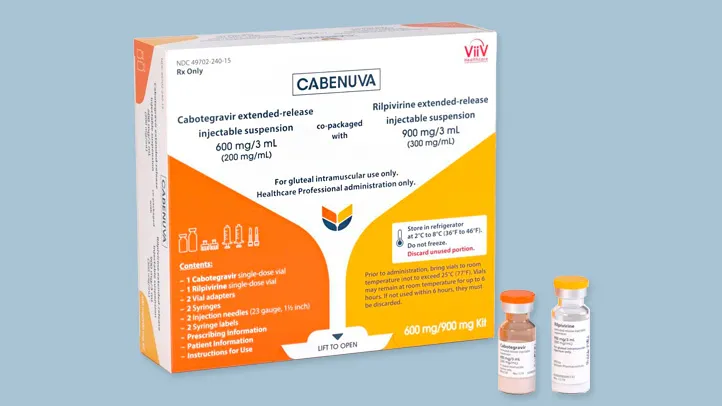
For decades, HIV prevention efforts have been loaded with issues—testing procedures, limited options for at-risk groups, and the nerve-racking complexity of existing treatments. The introduction of LEN into the suite of HIV prevention tools can be seen as a decisive action aimed at bolstering these efforts. Alongside daily oral PrEP, injectable cabotegravir, and the dapivirine vaginal ring, LEN is emerging as a must-have addition to the HIV prevention toolkit.
This diversified approach to HIV prevention is critical because it provides individuals with choices that better fit with their lives. Regimens in the field of HIV care are often riddled with tension and confusing bits, especially when it comes to daily adherence. By significantly reducing the intervention frequency, LEN not only simplifies the process but also reduces the intimidating responsibility of remembering a daily dose.
In addition, lenacapavir is helping to break down barriers that have long hindered effective HIV prevention. By providing an alternative that is far less invasive in terms of daily management, LEN caters to populations that have long been underserved by traditional HIV therapies.
Community-Centric Implementation: Overcoming Access Barriers
A critical component of the new guidelines is the emphasis on community-based delivery. Health authorities are now advocating for a more public health–oriented approach to HIV testing that makes use of rapid diagnostic tests. This strategy is particularly important because it enables easier access to LEN and other long-acting PrEP solutions through venues like community pharmacies and clinics, as well as tele-health services.
This shift towards community-centric implementation is designed to tackle the scary parts of traditional health care delivery. By eliminating complex, costly procedures, the guidelines ensure that vulnerable groups will no longer have to face overwhelming administrative hurdles to receive care. Simplifying testing protocols means that the process becomes more accessible and manageable, reducing the nerve-racking concerns that have plagued HIV prevention efforts in the past.
Key measures recommended include:
- Streamlined testing procedures using rapid HIV tests
- Decentralized delivery of long-acting injectables in community centers
- Tele-health consultations to support and monitor adherence
This strategy not only makes it easier for individuals to get tested but also facilitates quicker access to effective prevention methods—essential for curbing the spread of HIV among high-risk groups.
Real-World Impact: Building a Robust HIV Response
The implementation of injectable LEN is not just a theoretical exercise—it has practical, real-world implications. With 1.3 million new infections reported in recent years and certain populations bearing the brunt of the epidemic, the introduction of LEN could significantly tilt the scales in favor of HIV prevention.
LEN is particularly crucial for individuals who have struggled with daily adherence due to factors such as stigma or limited access to health care. This long-acting formulation addresses these complicated pieces by reducing the frequency of administration, offering a solution that is both effective and minimally disruptive to daily life.
The potential benefits of LEN extend beyond individual health outcomes—it represents a key public health tool. Health professionals now have an opportunity to figure a path toward improved HIV prevention strategies that rely less on the nervous routine of daily medication and more on scheduled, periodic injections that offer theoretical full-year coverage.
Integrating HIV Services with Broader Health Care
One of the most important developments in this new phase of HIV prevention lies in the integration of HIV services with other health care initiatives. By incorporating screening and management of noncommunicable diseases (NCDs) such as hypertension and diabetes, as well as mental health support, the guidelines propose a more holistic approach to patient care.
This integration is key in addressing the fine points of overall health care. By combining HIV prevention with other critical health services, the strategy not only enhances the uptake of HIV prevention tools like LEN but also promotes better overall health outcomes. The new recommendations encourage health care providers to offer consolidated services that cater to the whole person, rather than addressing health issues in isolation.
Benefits of a unified health care approach include:
- Improved access to medical services beyond HIV prevention
- Enhanced monitoring of patient adherence and health outcomes
- More efficient use of limited health care funding
- Reduced administrative hurdles by consolidating care provision
This framework is particularly promising for key populations who often face multiple, simultaneous health challenges. Coordinated care, where services are integrated across various medical fields, ensures that patients receive more balanced and effective treatment options.
The Role of Stakeholders in Expanding Access
Effective implementation of LEN requires coordinated support from governments, non-government organizations (NGOs), donors, and global partners. An essential part of this journey is ensuring that every one of these stakeholders understands the hidden complexities and fine details of the new guidelines.
Governments, for instance, are urged to integrate LEN into their national HIV prevention programs. This means ramping up procurement processes, training health care workers on the new protocols, and launching public awareness campaigns to educate communities about the benefits of long-acting PrEP.
Similarly, NGOs and community organizations are called upon to play a proactive role in both disseminating information and addressing the subtle differences in individual attitudes toward HIV prevention. Their community networks are invaluable in bridging the gap between policy and practice, especially in remote or underserved regions.
Key stakeholder responsibilities include:
- Policy formulation that incorporates LEN into national health agendas
- Capacity building for health care workers on new administration techniques
- Public education campaigns to demystify the benefits of injectable LEN
- Data collection and analysis to monitor real-world impacts
Such concerted efforts can help steer through some of the nerve-racking parts of policy implementation. With the right support systems in place, the adoption of LEN can quickly become a cornerstone of global HIV prevention strategies.
Challenges and Opportunities in Implementation
While the promise of LEN is exciting, its implementation is not without challenges. The process of rolling out a novel treatment option is full of problems and can be intimidating for health systems already dealing with resource constraints. In addition, the task of training large numbers of health care providers and refining testing protocols presents its own set of twists and turns.
However, these challenges also carry opportunities. The reduced frequency of injections compared to daily oral pills presents an opportunity to reallocate resources to other critical areas in the fight against HIV. This includes investments in community outreach and health care infrastructure, which can be improved as LEN becomes more widely adopted.
The following table outlines some of the key challenges and the opportunities they present:
| Challenge | Opportunity |
|---|---|
| Training Health Care Providers | Invest in continuous education, leading to improved overall health care delivery |
| Adapting Rapid Testing Protocols | Promote a streamlined, community-focused testing model that simplifies access |
| Managing Limited Health Care Resources | Innovative resource allocation that maximizes outreach and service efficiency |
| Overcoming Stigma and Misinformation | Enhanced public awareness campaigns and community engagement to educate at-risk populations |
By taking a closer look at these dimensions, it becomes evident that while the task ahead is full of problems, the potential benefits far outweigh the risks. With strategic planning and comprehensive public health initiatives, even the most intimidating challenges can be overcome.
Addressing Testing and Diagnostic Hurdles
A major barrier to expanded HIV prevention has been the reliance on intricate and costly testing procedures. The new guidelines recommend a public health model that employs rapid HIV testing for the efficient delivery of long-acting injectable PrEP. This simplified testing protocol is a game changer for both health care providers and recipients.
By removing cumbersome diagnostic steps, patients can quickly and easily get the confirmation they need to begin treatment. It’s a shift from a nerve-racking process involving multiple laboratory visits to a streamlined, community-based screening process.
The practical benefits include:
- Faster turnaround times for test results
- Reduced costs associated with traditional testing methods
- Greater accessibility in community centers and non-traditional clinical settings
This approach not only makes it simpler for individuals at risk of HIV to access care, but it also alleviates the heavy burden on centralized health care facilities. The ripple effect is a more agile and responsive HIV prevention system that can quickly adapt to evolving public health challenges.
Community Engagement and the Path Forward
Community engagement is the linchpin for successful implementation of any public health initiative. In the case of injectable LEN, communities play an indispensable role in ensuring that information is disseminated accurately and that support systems are in place for vulnerable populations.
Local organizations, community leaders, and health advocates must work together to overcome the confusing bits and fine details of this new preventative measure. People often feel overwhelmed by the nerve-racking choices associated with traditional HIV prevention methods, and community-driven approaches can offer much-needed reassurance and guidance.
Effective community engagement strategies include:
- Organizing local seminars and educational workshops
- Utilizing social media platforms to spread awareness and share success stories
- Developing peer support networks that foster open dialogue about HIV prevention
- Incorporating feedback from community members into policy adjustments
These approaches help to create a support network that not only makes it easier for individuals to get around the often intimidating health care system but also ensures that preventive measures such as LEN are understood and embraced by the communities that need them most.
Lessons from the Past: Adapting to a Changing Global Health Landscape
Historically, the global health arena has been full of problems when it came to HIV prevention. The emergence of LEN is a step forward in a series of crucial breakthroughs that have reshaped the way health care providers approach HIV treatment and prevention. Past experiences have underscored the value of simplicity in managing treatment regimens, and LEN builds on that legacy by offering a more straightforward, less nerve-racking approach to HIV prevention.
This moment invites a comparison to previous transformative shifts in public health. From the rapid rollout of antiretroviral treatments to the integration of community-based care, history shows how innovations can drive tangible improvements in reducing infection rates and improving quality of life for millions. LEN, with its twice-yearly dosing schedule, appears poised to join this legacy of revolutionizing HIV care.
There are several key lessons from past public health interventions that are relevant here:
- Simplification of Protocols: Reducing the tangled issues and complicated pieces associated with daily medication enhances adherence and treatment success.
- Community Empowerment: Engaging local groups and health networks helps address the subtle parts of mistrust and misinformation.
- Integration with Broader Health Services: Combining HIV prevention with broader health care services ensures that interventions are comprehensive and effective.
- Robust Data Collection: Monitoring real-world outcomes allows for timely adjustments and improvements in treatment protocols.
It is incumbent upon the global health community to take these lessons to heart, ensuring that the rollout of LEN is as effective in practice as it is promising in theory.
Long-Term Implications for Global HIV Prevention
Injectable lenacapavir stands as a beacon of innovation, one that could redefine future approaches to HIV prevention. Its success has the potential to trigger a ripple effect—a shift from a reactive to a proactive model of managing HIV, where prevention takes center stage.
Looking at the long-term picture, the key implications include:
- Reduced HIV Incidence: Fewer daily worries about adherence can lead to lower rates of new infections.
- Enhanced Public Health Infrastructure: Expanding community-based testing and treatment hubs creates a more resilient health care network.
- Empowered At-Risk Populations: With more simplified testing protocols and injectable options, individuals gain greater control over their health.
- Global Health Equity: Broadening access to cutting-edge prevention strategies paves the way for more equitable health outcomes across regions.
These long-term benefits are super important because they not only help curb the spread of HIV but also strengthen overall public health systems. As countries roll out LEN, gathering real-world data becomes essential to refine strategies and address any hidden complexities in the implementation process.
Balancing Innovation with On-the-Ground Realities
While the promise of LEN is undeniable, deploying this new intervention in the real world involves managing your way through some overlapping challenges. The health sector already contends with resource limitations and regional disparities in access to care. Consequently, the rollout of LEN must be paired with a dose of realism and careful planning.
The process requires a balance between harnessing transformative innovation and addressing everyday hurdles such as:
- Workforce Training: Developing the skills necessary for safe and efficient administration of injectable therapies.
- Supply Chain Efficiency: Creating robust distribution channels to ensure that LEN is available where it is most needed.
- Community Outreach: Tailoring communication strategies to address local concerns and debunk myths about new treatments.
- Monitoring and Evaluation: Implementing stringent data collection protocols that allow for continuous improvement and adaptation.
In practice, modernizing HIV prevention is as much about deploying innovative tools as it is about reinforcing the underlying structures that support public health. By finding your path through these everyday challenges, health care systems can maximize the benefits of LEN and further the overall goal of ending the HIV epidemic.
A Call for Bold, Equitable Implementation
The introduction of injectable lenacapavir is a call to action for policymakers, health care professionals, and community leaders around the globe. Bold implementation of these innovative guidelines, grounded in a commitment to equity, is key to translating scientific breakthroughs into measurable public health gains.
As Dr. Tedros Adhanom Ghebreyesus and Dr. Meg Doherty have emphasized, the time to act is now. In an era marked by limited funding and evolving health care challenges, every stakeholder has a responsibility to ensure that advances such as LEN do not remain confined to clinical trials but extend to every community in need.
This means investing in community-driven health initiatives, streamlining testing protocols, and ensuring that local health care workers are well-equipped to handle this new therapy. It also involves aligning global policy decisions with on-the-ground realities, so that when innovative treatments hit the market, they empower communities rather than adding another layer of complicated pieces to an already intense situation.
Conclusion: Steering Toward a Future Free of HIV
Injectable lenacapavir offers a glimpse into a future where HIV prevention is simpler, more effective, and truly accessible to all. By replacing the nerve-racking daily pill regimen with a twice-yearly injection, this breakthrough is set to change the HIV prevention landscape—reducing the confusing bits and allowing individuals, communities, and entire health systems to focus on long-term wellbeing.
As we collectively work through the twists and turns of a complex global health environment, the promise of LEN reminds us that progress is possible. It is an invitation to take a closer look at our current systems, dig into the nitty-gritty of how we manage care, and ultimately build an HIV response that is as dynamic and innovative as the science behind it.
For communities burdened by the overwhelming challenges of traditional HIV prevention methods, the introduction of LEN offers hope—a rebuke to the tangled issues that have long hindered progress. As we move forward, the real measure of success will be seen in the reduced infection rates, improved quality of life, and a world where access to cutting-edge prevention and treatment is a given, not an exception.
The time has come for all stakeholders—governments, health care professionals, NGOs, and community advocates—to embrace this groundbreaking shift in HIV prevention strategies. Through coordinated, equitable, and bold action, we can transform the landscape of HIV care and pave the way toward a future where HIV is no longer a looming threat.
In summary, injectable lenacapavir is not simply an addition to the arsenal against HIV—it is a quiet revolution. By offering a more manageable, twice-yearly preventive treatment, it addresses many of the nerve-racking challenges that have plagued HIV prevention for decades. With its promise of simplicity, enhanced accessibility, and robust public health benefits, LEN is poised to become a cornerstone of global HIV strategies, guiding us toward a future free of HIV.
Originally Post From https://www.who.int/news/item/14-07-2025-who-recommends-injectable-lenacapavir-for-hiv-prevention
Read more about this topic at
The Drug That Could Revolutionize the Fight Against H.I.V.
Innovations in HIV Prevention