Reflections on Data-Driven Healthcare and Digital Transparency
In today’s fast-changing digital world, where even academic journals deploy essential cookies and privacy statements, it is hard to ignore the impact that digital transparency has on our understanding of health research. As we figure a path through the confusing bits of digital data collection policies and patient privacy guidelines, we are also reminded of the equally tricky parts of managing healthcare information in our clinical practices and research publications.
Many readers are familiar with the long, detailed disclosures that explain how every device is being tracked, what personal data may be stored, and how this information aids in developing tailored content or advertising. The cookie consent messages that we see on scholarly websites are not far removed from the layered process of understanding the outcomes of health interventions in medical science. When we get into the nitty-gritty of both digital transparency and clinical research, clear and patient-focused communication remains critical. It is a reminder that modern healthcare – whether delivered in person or over digital platforms – is continually evolving toward greater clarity and accountability.
The Role of Pain Science Education in Osteoarthritis Management
Recent research on pain science education (PSE) and exercise interventions for individuals with knee or hip osteoarthritis presents an interesting case study. As outlined by a systematic review published in a reputed journal, the integration of educational sessions designed to reframe patients’ pain perceptions is now seen as a promising complement to exercise therapy. This approach is emerging as a critical element in preoperative rehabilitation, especially for patients awaiting total knee or hip replacement.
At its core, PSE is designed to address beliefs about pain that can create nerve-racking, overwhelming impressions. By challenging these misconceptions, practitioners can help patients better understand that pain does not always equal damage. Approaches that directly tackle the tangled issues surrounding pain are being seen as not just beneficial to relieving physical symptoms but also in addressing psychological obstacles that prevent patients from engaging in healthy physical activity.
This area of research has drawn a broad spectrum of opinions from practitioners and healthcare policymakers alike. On one hand, the perceived benefits of PSE in reducing detrimental beliefs such as pain catastrophizing, kinesiophobia (fear of movement), and low self-efficacy are recognized as essential components of a comprehensive treatment plan. On the other hand, the effectiveness of PSE when delivered as a standalone intervention appears limited, highlighting the need to pair education with structured exercise to truly reshape patient outcomes.
Key Components of Pain Education Interventions
When we dive into the fine points of pain science education interventions, several core educational domains emerge. Each of these domains aims to educate patients about pain physiology, chronic pain mechanisms, and strategies to maintain and improve physical function. The systematic review identified six major domains:
- Introductory Topics: Establishing fundamental concepts about what pain means and how it is experienced in a physiological context.
- Acute Pain Mechanisms: Understanding the short-term pain response and its role in injury and recovery.
- Chronic Pain Mechanisms: Exploring how prolonged pain can alter neurological pathways and impact long-term wellbeing.
- Factors That Sustain Pain: Addressing the confusing bits of psychological and lifestyle factors that contribute to persistent pain experiences.
- Multidisciplinary Education: Emphasizing the need for integrated knowledge from various health care disciplines.
- Exercise Components: Combining physical activity with education to boost overall outcomes and encourage self-management.
Understanding these six domains and their individual impacts on outcomes, such as pain reduction and physical functioning, is super important. However, one must also consider how these instructional elements interact with each patient’s personal experience of pain, making the design of interventions both challenging and exciting.
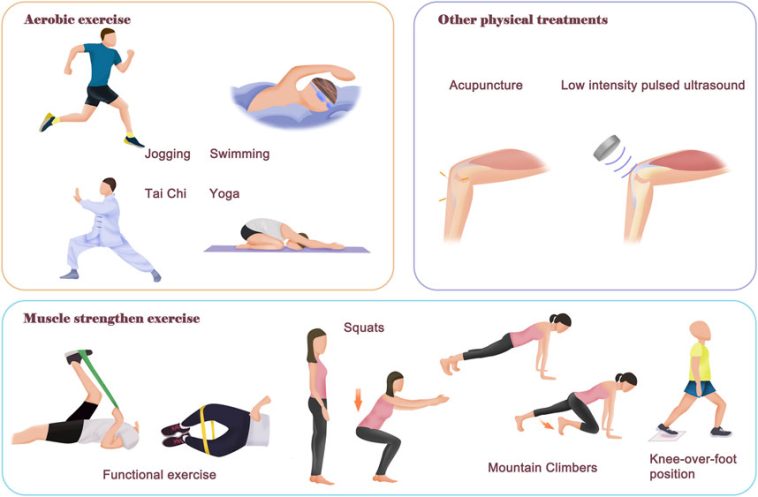
Digging Deeper into Exercise Interventions Amid Osteoarthritis
An equally compelling piece of this dialogue is the role of exercise therapies in complementing pain science education. Exercise is widely recognised as a must-have element in managing osteoarthritis symptoms, yet the barrier of pain can make such activity seem intimidating to many. The real success of these interventions depends on the delicate balance between addressing psychological factors and the physical regimens prescribed.
Many patients report that the twist and turn of self-doubt when faced with the challenge of physical activity is overwhelming. Yet, research indicates that when patients’ fears and misconceptions are addressed upfront through PSE, the path to a structured exercise program becomes smoother. The idea is to instill confidence and build self-efficacy, encouraging patients to follow through with the exercise programs despite the initially scary reputation of strenuous physical activity.
This integrated approach is also noteworthy because it demonstrates that effective therapeutic regimens need to be customized. Tailoring exercises in a way that resonates with patients’ everyday experiences alleviates some of the nerve-racking concerns they have about movement. When the rationale for each exercise is clearly communicated through relatable examples, the fine shades between what is damaging and what is healing become clearer. Thus, patients are better equipped to engage actively in their care.
How Tailored Exercise and Education Work Together
It is true that the relationship between pain education and exercise is more than just a simple addition of two therapies—it is about integrating them so that each supports the other. Here are some of the subtle parts of this integrated approach:
- Personalization: Tailored programs ensure that patients get a routine that suits their physical capabilities and mental attitudes toward pain.
- Bridging the Gap: Education sessions help explain why exercise is beneficial even if it appears nerve-racking at first, easing the transition from pain avoidance to active participation.
- Enhanced Self-Efficacy: When patients witness improvements in physical functioning, it reinforces their belief that they can manage their pain effectively.
- Reduced Catastrophizing: By directly addressing the tangled issues behind their pain, patients may experience reduced anxiety and fear about their condition.
There is an emerging consensus that pain science education is more successful when delivered with concrete examples and relatable exercises. This synergy between education and physical activity is critical in helping patients find their way through the daunting challenge of managing osteoarthritic pain.
Challenges and Opportunities in Digital Health Research
The same way that clinical interventions face tricky parts in patient care, digital research environments are filled with their own tangled issues. When scholarly articles and online journals present extensive descriptions about cookie policies and data privacy, it may initially seem overwhelming for the average reader. However, these disclosures play a key role in ensuring transparency and protecting personal data.
For example, a lengthy privacy notice may seem off-putting at first glance, but it actually outlines the ways and means by which data is stored and accessed by researchers and commercial partners alike. This transparency is crucial in an era where data breaches or misuse of personal information could have far-reaching consequences. Just as clinicians need to address the overwhelming fears in patients’ minds, researchers need to take the time to walk through the defensive layers built around digital data and emphasize trust in the process.
Digital health research is most effective when patients feel safe sharing sensitive information that can ultimately lead to better-tailored treatment protocols. When the responsibility for managing personal data is taken seriously, it builds rapport and trust. This trust is a must-have ingredient in a successful healthcare strategy, reinforcing the need for clear and straightforward privacy policies that support research transparency.
Understanding Data Privacy and Its Impact on Patient Engagement
Let’s break down some of the key points related to digital transparency and how they contribute positively to healthcare research:
- Information Storage: Explains how cookies and online identifiers are used to store information that can help personalize the user’s experience, which indirectly supports more tailored research outcomes.
- User Consent: Outcomes of clear consent choices help ensure that users are aware of how their data may be used, sustaining trust between the platform and the user.
- Data Protection: With varying standards across regions, particularly outside the European Economic Area, robust mechanisms must be in place to protect sensitive data.
- Ongoing Updates: Regular updates to privacy policies serve as a reminder that the digital landscape is in constant flux—a subtle detail that reinforces the importance of keeping data policies current.
These considerations serve as a bridge between research ethics and everyday user experience. Just as clinicians need to tailor their approach to ensure patient understanding, digital platforms need to manage their content in a way that the average reader can easily get around the intimidating language of legal jargon. In doing so, both health practitioners and researchers support an environment built on trust and mutual respect.
Wait Times and Economic Pressures in Joint Replacement Procedures
The ongoing pressures on healthcare systems in providing timely joint replacement surgery add another layer of complexity to patient care. Recent reports have shown that waiting lists for knee and hip replacements remain a significant issue across many regions, particularly in the wake of the COVID-19 pandemic. These economic pressures, combined with the confusing bits of waiting times and logistical delays, can contribute to a deterioration in patient well-being.
Patients often find themselves stuck in a loop of uncertainty, where every new day might carry the burden of intensified pain or the overwhelming fear of deteriorating mobility. In fact, many patients describe the period of waiting as a nerve-racking experience full of problems that extend far beyond just the physical symptoms of osteoarthritis. The possibility of worsening pain and functional decline during this period further underscores the need for effective, immediate interventions that combine pain science education with exercise regimes.
Integrating PSE with early-stage exercise programs offers a promising way to mitigate this challenge. By addressing not only the physical symptoms but also the psychological twists and turns that accompany chronic pain, these interventions may help patients feel better prepared to tackle the wait for surgery. Clear communication about the goals of therapy and the potential benefits can also help patients set more realistic expectations, ensuring that they are better equipped to manage their symptoms during this nerve-racking waiting period.
Addressing the Tricky Parts of Managing Patient Expectations
There are several subtle details that healthcare providers must consider when managing the psychological and practical aspects of long surgical wait times:
- Open Communication: Transparent dialogue about what patients can expect while on the waiting list can ease fears and reduce uncertainty.
- Preoperative Conditioning: Programs that integrate PSE with physical conditioning not only prepare patients for surgery but also build self-confidence.
- Resource Allocation: With stretched healthcare budgets and increasing demand, optimizing resources to deliver both education and exercise is critical.
- Long-Term Planning: Strategically planning interventions that span from preoperative to postoperative phases ensures continuity in patient care and recovery.
Healthcare systems must work through these challenging bits by prioritizing patient-centered strategies. By integrating educational programs that address both the physical and psychological aspects of pain, practitioners have a better chance of reducing the negative impact of prolonged wait times. This approach also highlights the need for further research into personalized intervention programs that cater to the unique experiences and expectations of each patient.
Embracing Integrated Approaches in Modern Clinical Practice
There is a clear emerging trend of working through the tense landscape of clinical management by integrating education with physical exercise. This integrated approach, which encompasses both pain science education and well-tailored exercise interventions, represents a promising way forward for the treatment of osteoarthritis. The systematic evidence shows that while PSE on its own may have limited effects on pain intensity or physical functioning, its critical role in reducing catastrophic thinking, fear of movement, and building positive self-belief cannot be underestimated.
It is essential that future research and clinical application take the vital step of personalizing these approaches. Combining the science of pain education with a strategic exercise regimen means that healthcare professionals are able to offer more comprehensive care. This combination not only helps patients better understand their conditions but also equips them with practical tools to manage both pain and functional limitations effectively. Ultimately, such a multifaceted approach can lead to improved outcomes in both preoperative and postoperative settings.
Synthesizing the Benefits for Comprehensive Care
When we try to untangle the interconnected issues of patient education, physical exercise, and healthcare system challenges, several key benefits emerge:
- Enhanced Psychological Wellbeing: By reducing negative thought patterns and instilling confidence, patients are more likely to engage fully in their treatment plans.
- Improved Physical Function: Tailored physical activity that is reinforced by robust educational components can lead to better postoperative recovery and long-term joint health.
- Effective Use of Healthcare Resources: Integrating multifaceted educational strategies may alleviate some of the pressure on overloaded healthcare systems by empowering patients to manage their conditions more effectively.
- Patient-Centered Care: Prioritizing clear communication, empathy, and personalization ensures that interventions are both meaningful and manageable for those living with osteoarthritis.
By synthesizing these benefits, it becomes apparent that bridging the gap between research and practice is more than just an academic exercise—it is a practical necessity. The success of integrated care models, combining the fine details of pain education with strategic physical activity, underscores the importance of continual innovation and adaptation in clinical practice.
Patient Empowerment Through Education and Evidence
While cutting-edge research lays the foundation for what may seem like intimidating interventions, the true impact of these approaches is measured in how empowered patients feel. When individuals are brought into the conversation through relatable examples that simplify the overwhelming aspects of their conditions, they are more likely to take ownership of their treatment. Pain science education, for instance, demystifies the nerve-wracking complexities of chronic pain and empowers patients by giving them a clearer understanding of their anatomy and the way their body works.
Empowerment comes not from medical jargon alone but from relatable, everyday language that patients can understand. Practical education sessions accompanied by guided physical activity sessions make the review of pain mechanisms less complicated, thereby allowing patients to get around their fears and actively participate in their recovery process. This approach transforms a nerve-racking journey into one of self-improvement and, ultimately, greater hope and commitment to the treatment process.
Strategies to Enhance Patient Empowerment
Here are several actionable strategies that can help bridge the gap between scientific evidence and patient experience:
- Use Relatable Examples: Incorporate real-life scenarios that resonate with everyday experiences, helping patients make sense of what might seem like convoluted scientific data.
- Simplify Communication: Replace academic or overly technical language with down-to-earth explanations, enabling patients to digest the key messages effectively.
- Personalize Interventions: Tailor both education modules and exercise routines to cater to the individual needs and abilities of patients, ensuring that each person feels a personal connection to their care plan.
- Encourage Active Participation: Foster a two-way dialogue where patients can share their concerns and successes, reinforcing their role in driving their own recovery.
Implementing these strategies can make a significant difference in patient outcomes. By focusing on making complex details understandable and accessible, providers not only boost patient confidence but also improve adherence to treatment plans. The positive cycle of education, empowerment, and improved physical function creates a win-win situation for both patients and healthcare systems.
The Economic and Social Implications of Integrated Pain Management
Beyond the direct clinical benefits, the integration of pain science education with exercise therapy carries substantial economic and social implications. Joint replacement procedures, particularly for knee and hip osteoarthritis, are becoming more common, which in turn places immense pressure on healthcare resources. The economic burden of prolonged waiting times and suboptimal preoperative management is loaded with issues that affect not just the individual patient but also society as a whole.
Innovative approaches that combine education with exercise offer a promising way to ease this burden. By reducing the negative psychological impacts of chronic pain, fewer patients may end up in a cycle of increased healthcare usage, including repeated consultations, prolonged medication use, and even the necessity for additional surgical interventions. More effective preoperative preparation could lead to faster postoperative recovery, reducing both the economic strain on hospitals and the indirect costs borne by society, such as lost productivity and long-term disability.
Moreover, the societal benefits of empowering patients through education are significant. When patients gain a clearer understanding of their conditions and learn to manage their own care, the ripple effect is felt in their families, workplaces, and communities. The potential for a broader positive impact on public health – one that extends far beyond individual clinical outcomes – is clear. This is why integrated pain management models are viewed as key investment areas for the future of healthcare.
Understanding the Ripple Effects on Society
Let’s take a closer look at some of the subtle details that underline the broader economic and social impact:
- Reduced Postoperative Complications: Enhanced preoperative education and conditioning can lead to smoother recoveries, lowering the risk of complications and thereby reducing hospital readmission rates.
- Improved Workforce Participation: When patients recover faster and experience less debilitating pain, they are more likely to return to work sooner, thereby boosting overall productivity.
- Lower Long-Term Healthcare Costs: Effective early interventions may prevent the escalation of osteoarthritis symptoms, reducing the need for expensive late-stage treatments.
- Enhanced Quality of Life: By addressing not only the physical but also the psychological facets of pain, integrated interventions contribute to a better overall sense of wellbeing, which has a positive impact on communities.
These points underscore the critical role that comprehensive pain management strategies can play in alleviating the broader economic and social challenges faced by our healthcare systems. By investing in methods that are both patient-centred and evidence-based, we can work through the tangled issues and create a sustainable pathway to improved public health.
Final Thoughts: Bridging the Gap Between Science and Everyday Application
The systematic review of pain science education and exercise interventions paints a picture of an evolving landscape where education meets enthusiasm for movement. The research clearly indicates that while PSE interventions may exhibit limited direct effects on pain and physical functioning when used by themselves, their essential role in improving psychological outcomes cannot be dismissed lightly. The ability to reduce fear of movement, improve self-efficacy, and diminish catastrophic thinking are all key benefits that support patient recovery both before and after surgery.
In an era where both scientific research and digital transparency are evolving hand in hand, the need for clear, relatable, and patient-centred interventions has never been more important. We must figure a path through the complicated pieces of clinical data, digital policies, and economic pressures by championing integrated approaches that treat patients holistically. Doing so means combining the fine details of pain science education with personalized exercise programs, all while maintaining a robust commitment to data privacy and patient engagement.
This integrated approach not only serves the immediate needs of patients awaiting joint replacement surgeries but also paves the way for more resilient public health strategies. By embracing the synergy between physical and psychological therapies, practitioners can help patients overcome the intimidating world of chronic pain and the challenges associated with long wait times in our strained healthcare systems.
Looking ahead, the future of healthcare depends on our ability to take a closer look at the subtle parts of both clinical and digital realms, ensuring that patients receive care that is as much about understanding as it is about healing. As research continues and technology evolves, the ultimate goal remains: to build a system where transparency, empathy, and science come together to transform the patient experience.
In conclusion, the journey toward a better integrated pain management system is very much like navigating through a thick forest of data, policy, and human emotion. We must keep our eyes open to the little details that matter, work through the nerve-racking challenges with both creativity and precision, and, most importantly, keep the patient at the centre of every decision we make. Only by doing so can we ensure that our evolving healthcare models are both effective and compassionate.
The path forward is not without its twists and turns, but it is one that offers immense promise. With ongoing research, improved digital practices, and an unwavering commitment to patient empowerment, the healthcare community is poised to redefine what it means to manage chronic conditions like osteoarthritis. As we continue to adapt to the ever-changing circumstances of both clinical practice and digital communication, one thing remains clear: a patient-focused, integrated approach is the super important way forward.
It is time to steer through the labyrinth of data-driven healthcare and make your way toward a future of transparency, efficiency, and, above all, compassionate care. Let’s commit to an improved partnership between digital innovation and clinical practice, ensuring that every patient finds the clarity and confidence they need to move forward on their journey to recovery.
Originally Post From https://bmcmusculoskeletdisord.biomedcentral.com/articles/10.1186/s12891-025-09313-4
Read more about this topic at
Educate. Exercise. Empower. | YSU
Educate. Exercise. Empower. Why Walk With a Doc? Initial …